In Brief
Investments in 5 key talent and technology areas can redefine acute care delivery
- Challenges across care, cost, and staffing are forcing healthcare organizations to rethink acute care delivery models.
- Precise organizational investments in both talent and technology areas can help reduce strain.
- Leading organizations are embracing staffing initiatives, including workforce redesign and top-of-license engagement, and technology, including predictive analytics, rounding, and virtual care.
As healthcare organizations seek to improve acute care delivery, challenges across staffing and technology threaten to neutralize progress. Gaps in either area would be complex enough individually; together, they create a formidable barrier between organizations and their ability to provide quality care and meet changing consumer preferences.
Hiring more staff to relieve bottlenecks and free up bed space is no longer a reliable path forward due to industry-wide burnout and inflated worker salaries, and the need for more technology investment and mounting cost pressures remain at odds.
Organizations looking to improve acute care delivery can do so with precise investments in modern staffing initiatives and specific technology areas.
Embrace new staffing initiatives and benefits
Consumers aren’t the only demographic asking for sweeping changes across healthcare. Discontent among workers is rising, with calls for change growing louder and more complicated for organizations to ignore. A full 81% of healthcare workers report feeling burned out in the last 6 months, up 17% from the previous year.
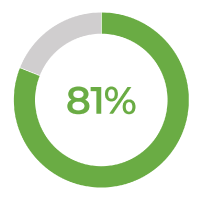
of providers, nurses, and non-clinical staff report feeling burned out in the last 6 months.
Without adequate staffing, patients everywhere will experience delays in care and a lack of access to the treatment they need—which means innovation can’t wait. For organizations seeking to improve acute care quality and patient outcomes, more attention must be paid to the workers providing that care. Investments in the following two areas can alleviate the burden placed on staff and ultimately provide them with the resources they need to meet patient demand.
Workforce redesign
Thoughtful redesign of clinical, ancillary, and support roles into a more team-based, patient-centric care model—with nurses functioning as coordinators of resources—marks a departure from a singular, department-driven approach.
Expanded skill portfolios should define roles across acute care (see chart), with each group taking on more responsibility within the scope of their expertise to free nurses to coordinate care, educate patients, and guide care progression. Traditional financial metrics such as hours per patient day (HPPD) will be challenged in this new care model, and alignment to a “cost-of-care” model will be required.
| Expanded roles of the future | |
|---|---|
|
Role Patient care support |
New responsibilities
|
|
Clinical care support |
|
|
Pharmacy |
|
|
Physical therapy |
|
Forward-thinking organizations are also relying on new technology levers to alleviate staff pressure, including re-recruiting RN’s who have left the workforce to educate newer nurses virtually and expanding virtual roles for staff when appropriate. Benefits of workforce redesign include:
- Increased worker satisfaction, leading to lower burnout rates.
- Stabilized staffing with less unplanned time taken off due to remote work.
- Improved patient engagement across different points of care, including admissions, discharges, and check-ins.
Top-of-license engagement
As cost pressures mount, healthcare organizations naturally look to do more with less and exhaust all available resources. However, that approach spreads staff too thin, contributing to higher rates of burnout and leaving fewer workers available to move patients through acute care.
Empowering clinicians to practice top-of-license continues to be a leading tactic—meaning clinical professionals’ routine tasks should utilize the full extent of their education, training, and experience, and tasks that could be performed by another worker should be performed by another worker. Benefits of top-of-license work include:
- Reduction in overall labor costs due to appropriate utilization of non-licensed personnel and thoughtful integration of students into care teams.
- Decrease in burnout due to staff not being overextended.
- Streamlined care delivery and throughput creating capacity for improved access to care.
The future of care delivery is here
As technology influences consumer preferences and shapes care delivery, the onus is on organizations to invest in scalable, patient-centric solutions. But urgency hasn’t always led to action; while organizations recognize digital transformation as essential to improving the consumer experience, financial concerns—among other factors—prevent necessary technology investments.
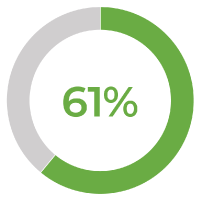
of healthcare organizations report that financial constraints prevent tech investments, up 31% from the prior year.
To improve acute care delivery, leading organizations are embracing a digital-first mindset and investing in the following core areas.
Predictive Analytics
Predictive capabilities have the power to change how healthcare is delivered. Leading organizations rely on access to accurate, real-time analytics across the entire patient population to:
- Detect acute disease early for at-risk populations.
- Analyze medical claims to proactively identify risk factors.
- Consolidate medical record data to prevent gaps in billing.
- Project admission, discharge, and transfer volumes.
Rounding
Building strong inter-staff and patient-staff relationships might seem more qualitative than quantitative, but data-driven rounding is essential for improving care delivery and efficiently moving patients through health systems. Technology-enabled rounding helps acute care staff to:
- Replace paper processes with simplified data collection and integration.
- Improve outcomes, predict clinical needs, and engage more deeply with patients.
- Address patient needs, improve monitoring, and support safety initiatives.
Virtual Care
As consumers demand more flexibility from organizations, it’s crucial that leaders look to integrate convenient and accessible virtual care solutions. Virtual care technology quickly connects patients with healthcare providers for services including consultations, diagnosis, and treatment, and can help acute care facilities by:- Freeing up available beds for patients that require in-person care.
- Enabling patients with tools to manage and improve their own health, improving chronic disease management and reducing readmissions.
- Supporting workforce alternatives that improve employee retention and job satisfaction efforts.
- Enabling a shift to alternative care delivery model that enables high-quality care with fewer resources.
As the strain on acute care facilities grows, the call for healthcare organizations to act becomes more urgent. Focused, precise investments in modern staffing initiatives and emerging technologies can not only create capacity and empower staff to provide better care, but can redefine acute care delivery for years to come.
